In the labyrinthine world of insurance, managing prescription drug claims can feel like wrangling a hydra-headed beast. Enter RxClaim: a powerful pharmacy benefits management (PBM) system poised to slay this multi-headed monster and bring order to the chaos.
What is RxClaim?
RxClaim is a comprehensive digital platform that automates and streamlines pharmacy claim processing for insurance companies, third-party administrators (TPAs), and corporate benefit plans. This cloud-based system tackles the complexities of:
- Claims Adjudication: Instantly verifies eligibility, formulary compliance, and pricing, resulting in faster payments and reduced errors.
- Benefit Management: Offers flexible benefit design options, including co-pays, deductibles, and tiers, to optimize cost-effectiveness.
- Rebate Management: Negotiates and tracks rebates from pharmacies and drug manufacturers, maximizing profit sharing and cost savings.
- Drug Utilization Review (DUR): Identifies potential medication conflicts and adherence issues, promoting patient safety and cost-containment.
- Data Analytics: Provides real-time insights into prescription trends, utilization patterns, and potential fraud, empowering informed decision-making.
RxClaim's Advantages:
- Reduced Costs: Streamlined processes, automated tasks, and improved data visibility lead to significant cost savings through efficient claim processing and optimized benefit management.
- Increased Efficiency: Real-time adjudication and improved workflows eliminate manual workload, allowing for faster turnarounds and improved productivity.
- Enhanced Transparency: Detailed data and reporting tools provide greater visibility into prescription trends, drug utilization, and potential fraud, facilitating informed decision-making.
- Improved Patient Care: DUR functionalities enhance patient safety by identifying medication conflicts and promoting adherence, while flexible benefit design options can cater to individual needs.
- Competitive Edge: RxClaim equips insurers and TPAs with the tools and insights to offer customized and cost-effective pharmacy benefits, attracting and retaining clients in a competitive market.
RxClaim in Action:
Imagine a health insurance company struggling with manual claim processing, high error rates, and limited data visibility. By implementing RxClaim, they achieve:
- Faster claim processing: Claims adjudicated in real-time, reducing turnaround times from days to minutes.
- Reduced errors: Automated eligibility and formulary checks minimize human error and overpayments.
- Cost savings: Improved benefit design and negotiated rebates result in significant financial savings.
- Improved patient care: DUR alerts identify potential medication interactions and non-adherence, prompting interventions to improve patient safety and outcomes.
- Enhanced competitiveness: The insurer can offer more flexible and cost-effective plans, attracting and retaining covered individuals and employers.
RxClaim: Beyond the Technicalities
RxClaim is more than just software; it's a partner in navigating the intricacies of pharmacy claims management. With its advanced functionalities, data-driven insights, and focus on cost-effectiveness and patient care, RxClaim empowers the insurance industry to operate with greater efficiency, transparency, and ultimately, deliver better value to all stakeholders.
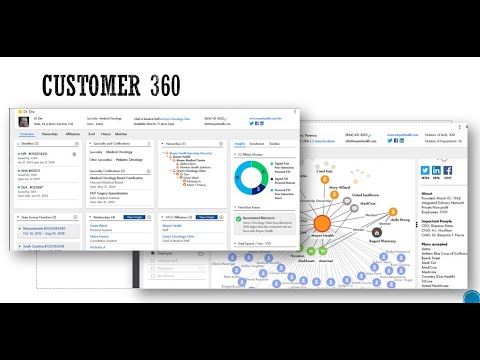
Learn how to onbard RxClaim data in Informatica MDM hub
No comments:
Post a Comment
Please do not enter any spam link in the comment box.